Anaemia
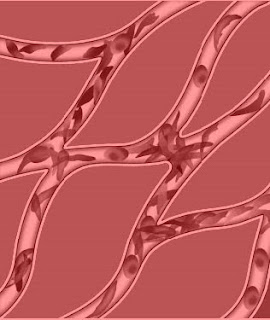
A reduction in the quantity of the oxygen carrying pigment “hemoglobin in the blood or may be defined as a reduction in the oxygen transport capacity of the blood”. Anaemia is the reduction of red cell mass and Hb concentration below normal levels resulting in impaired oxygen delivery to the tissues.
 Classification
Classification
1) Due to diminished production of normal red cells
i) Deficiency of Iron
• Nutritional
• Post-hemorrhagic
• Malabsorption
• A failure of iron utilization rather than deficiency
ii) Deficiency of B12 or Folate
• Pernicious anaemia
• Nutritional
• Due to disease of gastrointestinal tract
• Anaemia in pregnancy
• Anaemia in infancy
• Due to various drugs
iii) Due to vitamin C
iv) Deficiency of Thyroxine
v) Aplastic Anaemia
2) Due to excessive blood destruction (Haemolytic Anaemia)
i) Hereditary spherocytosis
• G6PD deficiency
• Sickle cell anaemia
• Thalassaemia
ii) Due to infective or toxic factors
iii) Due to Erythrocyte Antibodies
• Hemolytic disease of newborn
• Autoimmune hemolytic anaemia
• Symptomatic Hemolytic anaemia
3) Anaemia of uncertain origin
• Anaemia associated with chronic infection
• Uraemia
• Rheumatoid arthritis
• Liver disease
• Malignant disease
General Clinical Features of Anaemia
1) Fatigue and lassitude
2) Breathlessness on exertion
3) Dizziness,
4) Dimness of vision
5) Headache
6) Pallor of skin and mucous membrane
7) Anorexia and dyspepsia
8) Tingling and pins and needle sensation in the fingers and toes
9) Oedema
10) Palpitation, tachycardia, cardiac dilatation, systolic murmurs.
Deficiency of Iron: Occurs mainly in women of child bearing age because of enhanced demand for iron resulting from blood loss from menstruation and increased nutritional requirements of pregnancy and lactation.
Clinical features: General clinical features, glossitis, angular stomatitis, koilonychia, atrophy of mucosa of the pharynx and stomach, sometimes giving rise to dysphagia. In severe and long standing cases spleen may be palpable.
Deficiency of Vit B12 and folic acid: Causes are
Dietary deficiency
Gastric factors: hypochlorhydria (deficiency of Hydrochloric acid).
In elderly patient or following gastric surgery can impair the release of vit B12 deficiency.
Pernicious anaemia: This is an autoimmune disorder in which gastic mucosa is atrophic with loss of parietal cells causing intrinsic factor deficiency. In absence of intrinsic factor less than 1% of dietary vitamin B12 is absorbed.
Small bowel factors: Pancreatic insufficiency / Crohn’s disease- cause vit B12 deficiency.
Causes of folate deficiency:
Poor intake of vegetables
Caeliac disease
Increased demand in pregnancy
Drugs eg-anti-convulsant, contraceptive pills interfere the absorption of folate.
Anaemia due to excessive blood destruction:
In acholuric jaundice (Hereditary Spherocytosis)
Symptoms usually appear in childhood but they are often insufficient to cause the patient discomfort.
Symptoms are:
Severe anaemia,
Jaundice,
Increased splenic enlargement,
Weakness
Breathlessness,
In severe cases, may be very marked and associated with rigors, fever and vomiting.
Glucose 6 Phosphate Dehydrogenase deficiency
Persons with G6PD deficiency normally enjoy good health but are liable to haemolysis if any of the incriminated drugs or foods is ingested. However, it must be emphasized that the haemolytic effect is related to the dose and will not be clinically detectable, if the amount does not exceed a critical level.
Thalassaemia (Cooley’s Anaemia)
A hereditary blood disease, there is an abnormality in the protein part of the haemoglobin molecule. The affected red cells cannot function normally, leading to Anaemia. Other symptoms include enlargement of spleen and abnormalities of the bone marrow.
Individuals inheriting the disease from both parents are severely affected (Thalassaemia major) but those inheriting it from only one parent are usually symptoms free (Thalassaemia minor)
In Ayurveda it is known as Pandu roga.
Definition: All the diseases in which the colour of the patient becomes pale or pandur varna is known as Pandu Roga. It is pitta pradhan Tridoshaja vyadhi.
Etiological Factors: Causes of Pandu roga are related to Ahara (dietietic habits), vihar (daily regimen) and nidanarthkar vyadhi means some diseases which leads to pandu.
Ahara: Food which contains more sour, bitter, salt taste, less sleep during night, more sleep during day time, excessive exerises, suppression of natural urges, excessive thinking, sadness and angerness.
Nidanarthkar rogas for e.g.
Krimi Roga (Worm infestation)
Amlapitta (Gastric ulcer)
Menorrhegia /Metrorrhogia (Mensotrual disorders) lead to Pandu roga directly.
Due to these causative factors, the agnis (enzymes responsible for digestion and metabolism) stop functioning properly and as a result ama (semidigested material) is produced. This ama being sticky in nature and gets lodged in the circulating channels (srotas) and prevents the nourishment of Dhatus which leasds to pandu roga.
Deficiency of iron and vitamins contents in food also leads to pandu roga directly.
Treatment
1) Samtarpaniya chikitsa or Snehan chikitsa –
A) Internal – medicated ghee i.e. Panchgavya ghritam, Draksha ghritam, Dadimadya ghritam, pathya ghritam- dose 10 gram ( two times a day). All ghritam nourish the body with Pitta shamanam.
B) External – Abhayanga helps to reduce the stiffness and fatigue of the body.
2) Shodhana mild virechana is the best treatment for elimination of pitta from the body.
3) Medicines( Shamana chikitsa) some of them are-
Dhatryarishtam,
Dhatryavaleha,
Drakshadi kashayam,
Drakshadi avaleha,
Punarnava mandoor,
Mandoor vataka,
Lohasava.
Diet: Depends upon the appetite. Patient has to give little quantity of food, but frequently.
Vegetable- fenugreek, lettuce, spinach, soyabean, sesame seeds, radish, tomato, onion, carrot
Dry fruits: raisin, almond
Fruits: Banana, block grapes, plums, strowberries, pomegranate, apple, sugarcane juice.
Milk: twice a day.
