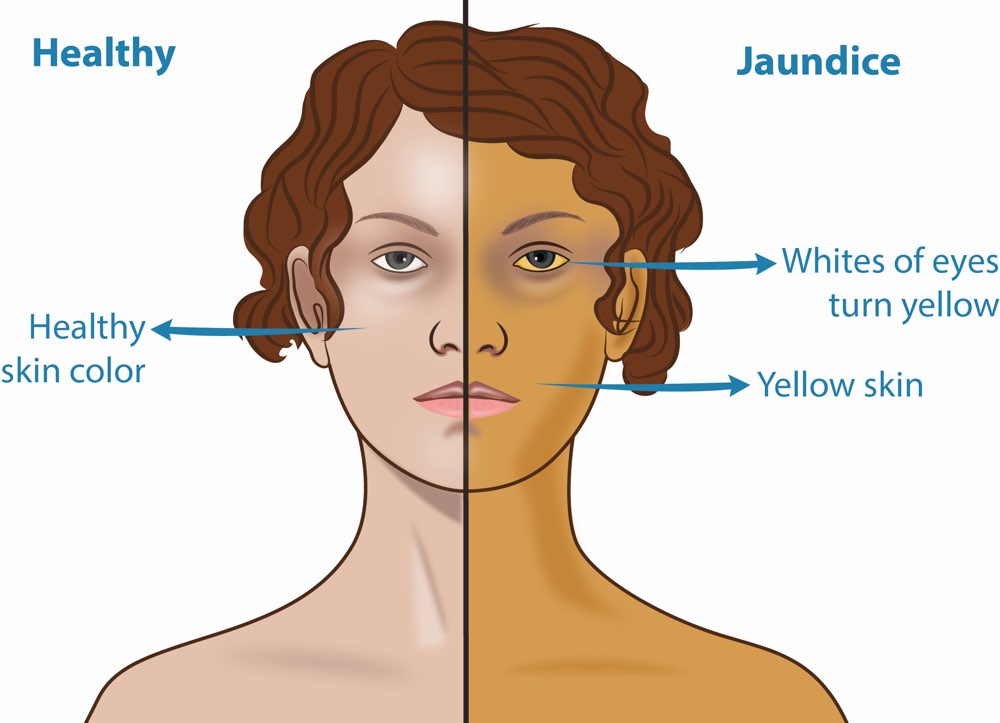
Jaundice
It is a clinical term referring to the yellowish discolouration of the skin, mucous membrane and whites of the eyes resulting from an increased bilirubin concentration in the body fluid. It is detectable when the serum bilirubin concentration exceeds 3mg/100ml less marked hyperbilirubinaemia is called latent jaundice. Jaundice is a sign rather than diseases that occurs in many diseases. According to the pathological variation Jaundice fall into 3 groups-
1) Haemolytic jaundice or Pre-hepatic: When there is excessive destruction of red blood cells in the blood causes the production of more bilirubin. Haemolysis may be due to intrinsic defects of the red blood cells or to various extra corpuscular factors. It is a mild one. Many patients have splenomegaly due to excessive activity of the reticulo endothelial system or congestion of the red pulp and also reticulocytosis and anaemia. The degree of anaemia depends on the severity of haemolysis.
2) Hepatocellular or Hepatic Jaundice: Results from inability of the liver to transport bilirubin into the bile as a result of liver cell damage, Acute paranchymal liver disease usually due to hepatitis A or B virus or to toxins, usually drugs or alcohol are common causes. Immature bilirubin transport mechanisms in the new born, especially n prematurity and congenital defects in bilirubin transport are very specific metabolic defects in the liver cell causing jaundice. The clinical features vary depending on the underlying diseases. Jaundice ranges from mild to very severe.
3) Obstructive or post hepatic jaundice: Obstruction to the excretion of bilirubin anywhere between the biliary canaliculus and Ampulla of vater may cause jaundice. Most common bile duct and carcinoma of head of the Pancreas. Other causes are
i) Carcinomas of the ampulla of Vater or bile duct
ii) strictures of the bile duct usually the result of previous surgery.
iii) Metastatic tumours impinging on the bile duct and
iv) very rarely involvement of common bile duct by a duodenal ulcer.
Symptoms are jaundice itself, if prolonged or severe may give the skin a greenish appearance, pale or clay colored stool due to deficiency of bilirubin and to steatorrhoea (increased amount of fat in faeces) and dark urine. In some patients there is generalized pruritus loss of appetite, metallic taste in the mouth, upper abdominal pain.
Jaundice in New Born
i) Physiological Jaundice
ii) Pathological jaundice
1) Physiological Jaundice: It usually appears after 30 hours, peak level of bilirbin is reached on the 4th or 5th day and icterus disappears by 7 days. It is due to immaturity of the liver during the first few days of life. Management is essentially symptomatic.
Causes are:
No specific therapy of physiological jaundice is required. The infant should be watched for any complicating illness or sudden rise of bilirubin level.
2) Phototherapy is used as an alternate metabolic pathway for degradation of bilirubin.
Pathological jaundice causes are:-
i) Excessive red cell destruction
• Rh incompatibility
• ABO incompatibility
• G-6 PD deficiency
• Pyruvate kinase deficiency
• Cephalhaematoma
ii) Metabolic factors
• Anoxia
• Respiratory distress
• Starvation
• Maternal diabetes
• Pyloric stenosis
• Drugs
iii) Mixed haemolytic and hepatotoxic disease
• Septicaemia
• Intrauterine infections such as cytomegalovirus toxoplasmosis,
• Rubella,
• Drugs
iv) Hepatocellular
• Neonatal hepatitis,
• Biliary atresia
Treatment: Consult the pediatrician and give the treatment according to the cause.
Jaundice is a key symptom of all forms of Hepatitis.
Hepatitis A virus – It is spread by ingestion of contaminated water and seafood’s (especially seafood) and is shed in the stool for 2 to 3 weeks before and 1 week after the onset of jaundice. Thus, close personal contact with an infected individual or faeco-oral contamination during this period accounts for most cases and explains the occurrence of outbreaks in institutional settings such as schools and nurseries.
Hepatitis B virus – It is the cause of ‘serum hepatitis’, is the most versatile of the hepatotropic viruses. Although blood and body fluids are the primary vehicles of transmission, virus may also be spread by contact with body secretions, such as semen, saliva, sweat, tears, breast milk, and pathogenic effusions. Transfusion, blood products, dialysis, needle stick accidents among health care workers, intravenous drug abuse constitute the primary risk categories for hepatitis B virus infection.
Hepatitis C virus – Parent rally transmitted, non A non B (NAN B) hepatitis has been known to cause 90 to 95% of cases of transfusion associated hepatitis the long search for the causative agent was rewarded in 1989 with the cloning of hepatitis C virus.
Hepatitis D virus – Also called the “delta agent” and “hepatitis delta virus” hepatitis D virus is a unique RNA virus that is replication defective, causing infection only when it is encapsulated by HBsAg.
Hepatitis E virus – is an enterically transmitted, water born infection occurring primarily in young to middle aged adults, sporadic infection and overt illness in children are rare.
In Ayurveda jaundice is known as kaamala. It is a sudha paitika roga. If a person has food which increases (aggravates) pitta, like excessive intake of sour, salty, spicy and oily food, excessive intake of alcohol, pitta becomes aggravated. It causes vitiation of Rakta and mamsa dhatu and leads to kamala Roga. Anaemic patient are more prone to kaamala.
Kaamala is classified into 2 types
• Shakha ashrita
• Kashtaashakhashrita
Laboratory tests:
Liver function test
Urine
Stool
Ultrasomography of abdomen
Modern treatment- Depends upon the symptoms of the patient.
According to Ayurveda: Kaamala is a pitta dominant (Pradhan) disease, so virechana is the best treatment to eliminate vitiated pitta from the body.
According to doshas aggravation, varieties of oral medicines are given to the patient.
Oral medication should be given for 3-4 months like:-
Drakshadi Kashayam
Vyoshadi Kashayam
Punarnavadi Kashayam
Vasa Guluchyadi Kashayam
Drakshadi leham
Rohitakarishtam
Amalaki Choornam
Other medicines which are good for liver rejuvenation.
Treatment should be done under doctor’s supervision.
Diet- Steamed leafy vegetables, rice, buttermilk, coconut water, juice (Apple, oranges), lot of water with lemon juice, barley water.
Avoid- Fried, fatty spicy and heavy food, non-veg.
Other recommendations are—
Take sufficient rest
Avoid excessive heat
Avoid stressful situations and anger
Cut down physical exertions
Keep diet rich in carbohydrates
No alcohol.

